Introduction: Insurance pooling in the context of CDIPC
Pooling is a system designed to bring stability to insurance premiums. It works by consolidating high drug cost claims from a large number of employers in order to share the risk and the cost of insurance. In this way, employers with recurring high drug claims are protected from the full impact of these claims by paying the pooling charge and not the full cost of drug claims. Similarly, employers with no high drug claims pay pooling charges and enjoy the peace of mind knowing they are protected in the event of high drug claims.
All Canadian life and health insurers that underwrite fully insured health or drug insurance plans are members of the Canadian Drug Insurance Pooling Corporation (CDIPC).
The CDIPC regime uses two pooling levels for paid claims by plan member or certificate – EP3 and industry pooling.
● The first level, known as EP3 pooling, shares drug costs among employer groups in the insurers pool commencing at a certain level or threshold as established by the insurer. An EP3 pool will pool claims up to the established industry pooling threshold (or Ongoing Threshold).
● When drug claim amount exceeds CDIPC’s Initial Threshold for two consecutive years it becomes eligible for CDIPC or industry pooling. Industry pooling covers 85% of the drug costs over the Ongoing Threshold up to the CDIPC pooling maximum.
EP3: What is it?
In 2012, in an attempt to standardize pooling approaches for drug claims, the CLHIA invited insurers to form a new type of pool called an EP3 (Extended Healthcare Policy Protection Plan) and administer EP3s in accordance with CDIPC standards. These standards are designed to bring affordability, availability and transferability of drug insurance coverage to employers’ benefit plans. Prior to 2012, each insurer governed their pools in accordance with their own guidelines.
EP3: How does it work?
Participating insurers must place all large drug claims, from all of their fully-insured group business, in a self-administered pool. Plan sponsors with fully insured benefit plans cannot opt out of being part of the EP3 pool their insurer places their benefit plan in.
Participating insurers cannot renew existing employers based on their own pooled drug claims experience, nor can they experience rate new business from another participating insurer based on that employer’s own pooled drug claims.
Insurers may, however, set premiums based on the experience of their entire EP3 pool, or based on other non-customer level experience criteria.
Drug and non-drug health benefits can be pooled together however;
● EP3 rules apply to the drug portion only of pooled benefits, and
● Insurers are required to have processes that can demonstrate that they are following EP3 rules for the drug portion. These processes are subject to annual compliance attestations and review by CDIPC.
All other aspects of the EP3 can be customized by participating insurers, including pricing, EP3 pooling threshold, and pooling approach (i.e. per certificate or per person insured, etc.). Insurers may also have multiple EP3 pools for different market segments if they choose. These approaches contribute to maintaining a competitive environment between insurers.
The “Industry” or CDIPC pool
The cost of Eligible Drug claims is shared by all participating insurers and is based on their share of total annual paid drug claims. This process is transparent and invisible to plan sponsors.
Industry pooling starts in the 2nd year of drug claims for a qualifying plan member that exceed the “Initial Threshold” for CDIPC coverage for that calendar year. This is also where EP3 pooling coverage by the insurer stops for plan members pooled under industry pool. The industry pools 85% of the plan member’s paid drug claims up to the CDIPC pooling maximum. Click here to see year by year thresholds and maximums.
Pooling and inflation
EP3 pooling helps create more sustainable drug insurance plans, by shielding employers from the full impact of their high drug cost claims. It’s important to note, however, that pooling cannot control or fully insulate plan sponsors against drug cost inflation and the proliferation of new high cost specialty drugs. What it does do is share financial impact from high cost drugs against a wider plan sponsor base.
The following example illustrates this concept:
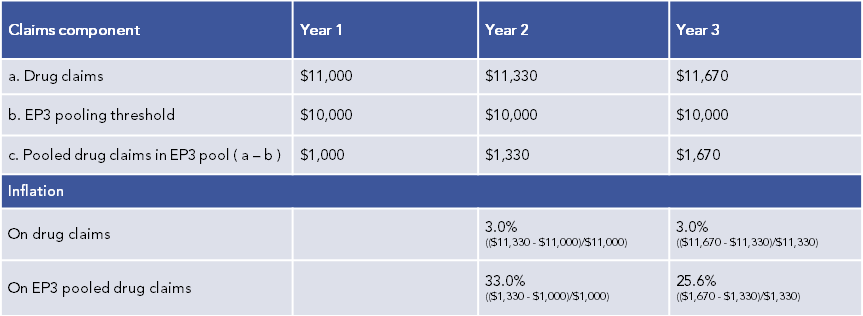
Regardless of CDIPC or EP3 pooling, the inflation in pooled claims each year is significantly higher than inflation on paid claims.
Pool integrity
Per CDIPC standards, if it is deemed that a group policy was created, in whole or in part, to bring together eligible certificates with high drug claims to take advantage of the pooling protection, the extended health benefit policy will be excluded from the EP3 and Industry Pool. This is to protect the integrity of the EP3 and CDIPC pool and avoid anti-selection.
New policies implementing an EHB benefit for the first time
Where an extended health benefit policy is issued for the first time (no prior coverage with another insurer) and a certificate’s claim costs were higher than the EP3 threshold at the end of the first policy year, insurers must audit the claims incurred on policy within six months of the first renewal to see whether any certificates had high pre-existing drug claims within the first benefit year.
Upon review, in the event that high pre-existing drug claims are found, insurers must retroactively remove the applicable claim costs from EP3 pooling for the period and include them in their LAP (Large Amount Pool) or an alternate insurance coverage and pricing mechanism. The certificate’s drug claims will continue to be excluded from the EP3 and pooled within LAP until they are less than the EP3 threshold for two consecutive benefit years.
Eligible drug claims for pooling
In order to be eligible, the certificate’s annual drug claims must be greater or equal to Initial Threshold for two consecutive years. In year three and in subsequent years, the drug Claim must be greater than the Ongoing Threshold.
To be eligible for EP3/CDIPC pooling, policies must not exclude specific certificates unless, as noted herein, specific pre-existing exclusion requirements are met. Insurers are also prohibited from experience rating policies in EP3 pools but can charge appropriate EP3 pooling charges.
If the fully insured policy existed and was in force prior to June 8, 2011; the policy was grandfathered into the EP3/CDIPC regime as an EP3/CDIPC eligible policy.
Fully insured that policies became eligible for pooling protection under an EP3 plan after June 7, 2011 and may have drug claims from certain certificates ineligible for EP3 and / or CDIPC pooling. This is to protect the EP3 & CDIPC pools from anti-selection. Per CDIPC’s rules, certificates should be deemed by the insurer to be “Excluded Certificates” if the insurance plan moved from an Administrative Services Only (ASO) or Refund accounting arrangement to fully insured after CDIPC started and the plan already had certificates that would qualify for EP3 and / or CDIPC pooling. Certificates deemed to be “excluded” will continue to be excluded from EP3 and/or CDIPC pooling until drug claims paid for the certificate are less than the Ongoing Threshold for two consecutive calendar years.
Click here for a table that provides greater detail on excluded certificates.
New employees, mergers or acquisitions, and spinoffs
Rules about pre-existing claims do not apply to employees hired after the EHB policy became EP3 eligible. In a merger or acquisition, rules about pre-existing claims do not apply if the purchased company had an EP3 under its own former EHB policy. If the purchased company was not eligible for EP3 pooling before the merger or acquisition, rules about the treatment of pre-existing claims will apply. This same logic applies to groups that split up in spinoffs.
Coordination with provincial drug insurance plans
Provincial legislation takes precedence over insurers’ EP3 pools. Any exclusions under an insurer’s EP3 apply only to the EP3 and not to provincial coverage. The drug pooling agreement will work in conjunction with provincial pooling arrangements, such as the Quebec Drug Insurance Pooling Corporation (QDIPC).
EP3 & CDIPC pooling risk to insurers and risk sharing
With this process, insurers still bear financial risk associated with high cost drug claims as noted below.
● 100% of claims in first year of occurrence
● 100% of claims portion under the Ongoing Threshold
● 15% of Eligible Drug claims over the Ongoing Threshold and under the Maximum Pooled Amount
● 100% of the claims portion over the Maximum Pooled Amount
● Insurers’ share of eligible drug claims in industry pool – based on industry pool experience
● All non-eligible claims
For an illustration of the EP3/CDIPC pool structure and financial risk to the insurer click here .

